Communication failures are the single most preventable source of medical errors, and these errors can have catastrophic consequences if they are allowed to occur. Interestingly, the aviation industry leads the charge when it comes to effective closed-loop communication. Consequently, the air medical transport industry is uniquely positioned to integrate the communication skills and practices from aviation into the world of patient care.
Closed-loop communication, a process of confirming the transmission of crucial information between two entities, plays a key role in patient safety and operational safety. Incorporating relatively simple communication techniques will reduce dangerous errors and delays, ultimately contributing to better patient care, better customer service, and better employee morale and long-term retention.
Download Poster
Communication:
- The imparting or exchanging of information or news;
- Means of sending or receiving information by various means
In an ideal world, communication is uncomplicated and effective every time information needs to be conveyed from one party to another. Given that the world of air medical transport is far from ideal, it stands to reason that communication within it also has room for improvement. Closed-loop communication is one strategy that absolutely upgrades safety, customer service, patient care, and employee morale—and it costs nothing more than simple behavior change.
While the aviation industry has long benefited from consistent loop closure, the medical industry lags. Prior to the COVID-19 pandemic, medical errors were the third-leading cause of death in the United States, right behind heart disease and cancer. And the number one source of medical errors? Miscommunication. As such, the air medical transport industry is uniquely positioned to integrate the communication skills and techniques from aviation into the healthcare environment.
To better understand what is meant by the term “closed-loop communication,” one only needs to imagine the back-and-forth between a pilot and air traffic control. A concise informational item is spoken by the pilot to ATC, and the disembodied voice from ATC comes across the radio repeating back exactly what was said as a means of confirmation. There are generally three elements in closed-loop communication: a sender of a message, the message itself, and the receiver of the message. When loop closure is performed perfectly, the sender states the message, the receiver echoes it back verbatim, and the sender of the message replies in the affirmative if the verbiage is correct. If the message is repeated back incorrectly, the sender of the message responds with a “No” or “Negative,” and restates the message correctly, and then waits for the receiver to close the loop correctly.
Interestingly, this aviation example omits nonverbal communication completely. However, studies indicate that anywhere from 65% to 93% of human communication is nonverbal, meaning that we primarily use facial expression, body language, and vocal features (such as tone, pace of speech, inflection, etc.)—everything other than the words themselves—to express the meaning of what is being said. Perhaps this is why text messaging can lead so easily to misunderstandings, and why emojis are so heavily used in order to ensure the sentiment of messaging is received accurately. Regardless, communication breakdown is often a huge source of conflict and disappointment in close interpersonal relationships.
Moving back to the medical transport industry, one could argue that effective workplace relationships are every bit as dependent on communication as are close interpersonal relationships. For the length of a shift, clinicians working together are in a committed partnership with each other and with their pilot and even the dispatchers. For the length of a transport, clinicians are in a committed relationship with their patient. For the length of a career, employees in the medical transport industry are in a committed relationship with their employer—each depends on the other, whether it’s for a paycheck, shift coverage, insurance, or retirement. Consequently, all of these relationships will benefit from better communication in order to avoid errors and misunderstandings, both of which could have fatal consequences when considered in the context of aviation and patient care.
Unfortunately, a closer look at the work environment reveals several features that make effective communication particularly challenging in this field. Air medical healthcare providers are typically tasked with performing patient care in the confines of a loud aircraft while wearing helmets with visors, COVID-era face masks on, physically separated from the pilot, and with both hands full of syringes, medications, IV catheters, and more. Meanwhile, communication with the dispatch center occurs via radio or satellite phone, and it might be broken or scratchy or poorly enunciated. Finally, in the big picture of employee-to-manager or employee-to-employer communication, email is the primary mode. In other words, nonverbal communication is essentially eliminated on the job. And because this represents well over half of all communication, the verbal component of communication becomes exponentially more crucial…it’s all there is!
Closed-loop communication begins with the sender of the message, who must ensure that the message being delivered is accurate, bold, and concise. The correct information is spoken clearly—not mumbled—and quickly gets to the point. In response, the receiver of the message must be timely—the reply should be immediate. It should also be specific, echoing the sender of the message exactly, and it should be certain, spoken with firm confidence to that the sender of the message has no doubt that the message has been received. Terminology and vocabulary should be standard and common for both the sender and the receiver based on the shared work environment.
It’s not difficult to imagine situations in which closed-loop communication might prevent catastrophic errors. An emergency response to the incorrect location causes a delay in patient care and has downstream effects on customer service. A communication breakdown between clinicians could lead to administration of the wrong medication or the wrong dose which clearly affects patient care. A misunderstanding during the transfer of patient care from one provider to another might result in malpractice. A manager who addresses an issue but never circles back to the employee who voiced it with a resolution will potentially lose that employee—or at least lose their faith and confidence. In the end, safety could be compromised, employee morale could suffer, and long-term employee retention will also become a challenge. Each of these scenarios has an enormous associated cost, and the dollar amount is probably the least of it.
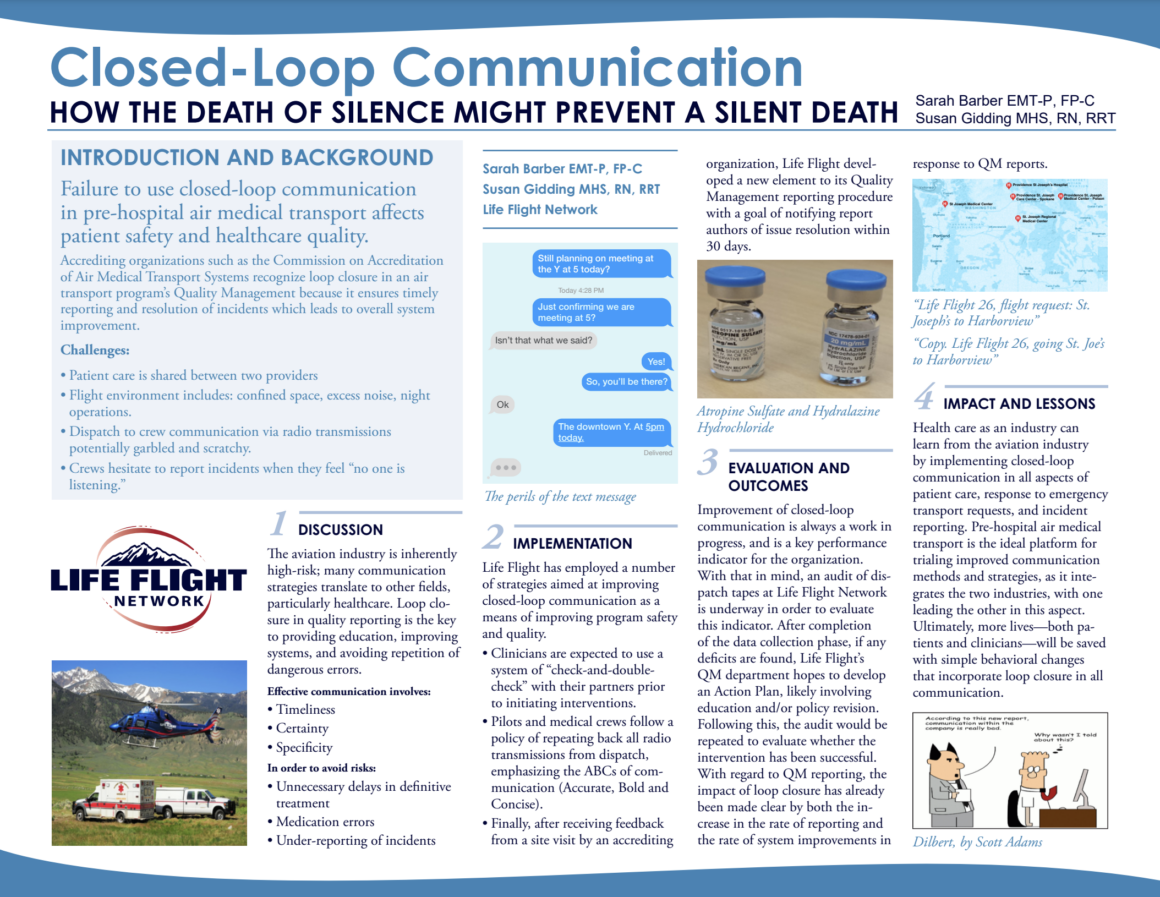
What Life Flight Network is doing to Close the Loop in communication
Consistent use of closed-loop communication is a habit that needs to form, and if taught well and monitored closely, it will. Several years ago, Life Flight Network began auditing a random 10% sample of communication between air medical response units (helicopters containing clinicians and pilots) and the dispatch center. It quickly became clear that closed-loop communication was not standard practice, as it was identified as present in only about 55% of calls (radio and/or satellite phone). An educational piece on the topic, along with a mandate, was delivered to all staff as an intervention, and calls to-and-from the dispatch center continued to be audited, allowing for feedback to staff. Within a few months, use of closed-loop communication rose to 95%–unambiguous evidence of a successful intervention strategy!
Similarly, Life Flight Network’s Quality Management Department developed a multi-faceted system to ensure loop closure for any employee addressing a concern with a Safety Report, a Quality Report, or an Employee Suggestion. Each type of incident report or suggestion goes through a formal investigation and evaluation process by various layers of management, including the CEO if necessary. When the issue has been resolved or the evaluation is complete, the author of the report receives an auto-generated email from the reporting system advising details of the resolution and encouragement to contact a direct supervisor if more detail is desired. This has led to staff feeling confident that their problems and ideas are being heard, which in turn improves morale and commitment to their organization.
Sarah Barber, EMT-P, FP-C
Quality Manager – Life Flight Network
sbarber@lifeflight.org
Presentations:
- AMTC 2019, CCMTC (Critical Care Medical Transport Conference) 2021
- Poster session presentation at the 2019 AAMC: Integrating Quality Conference (AAMC is the Association of American Medical Colleges).
- Taught as part of Life Flight Networks ‘Crew Resource Management’ training
References:
- Baker DP, Salas E, King H, et al. The role of teamwork in the professional education of physicians: current status and assessment recommendations. Jt Comm J Qual Patient Saf 2005; 31(4):185-202
- Institute for Healthcare Improvement: A Framework for Safe, Reliable, and Effective Care
- Mehrabian, A. (1972). Nonverbal Communication. New Brunswick: Aldine Transaction
- National Patient Safety Foundation: Free From Harm Accelerating Patient Safety Improvement Fifteen years after to Err is Human. 2015
- TeamSTEPPS Team Strategies & Tool to Enhance Performance & Patient Safety
- The Joint Commission: Sentinel Event Alert, Issue 58, September 12, 2017
- To Err is Human – Building a Safer Health System: IOM 2000. National Academy Press, Washington D.C.